PH-ILD Screening
Early PH evaluation may improve ILD patient outcomes, as an approved therapy is available.
A modified Delphi study was conducted to determine screening strategies for pulmonary hypertension in patients with interstitial lung disease using expert consensus.
Conclusion
Routine ILD clinical evaluations can trigger suspicion of PH, allowing for evaluation of additional tests including echocardiography and PH confirmation with a RHC
Pulmonary Hypertension Diagnostic Criteria for ILD Patients
1 Triggers for PH Screening in Routine ILD Evaluations
Panelists reached consensus on several triggers raising the suspicion for PH including:
-
Symptoms
-
Clinical signs
-
Chest CT scan findings or other imaging
-
Pulse oximetry abnormalities
-
6MWT worsening unexplained in pulmonary function tests
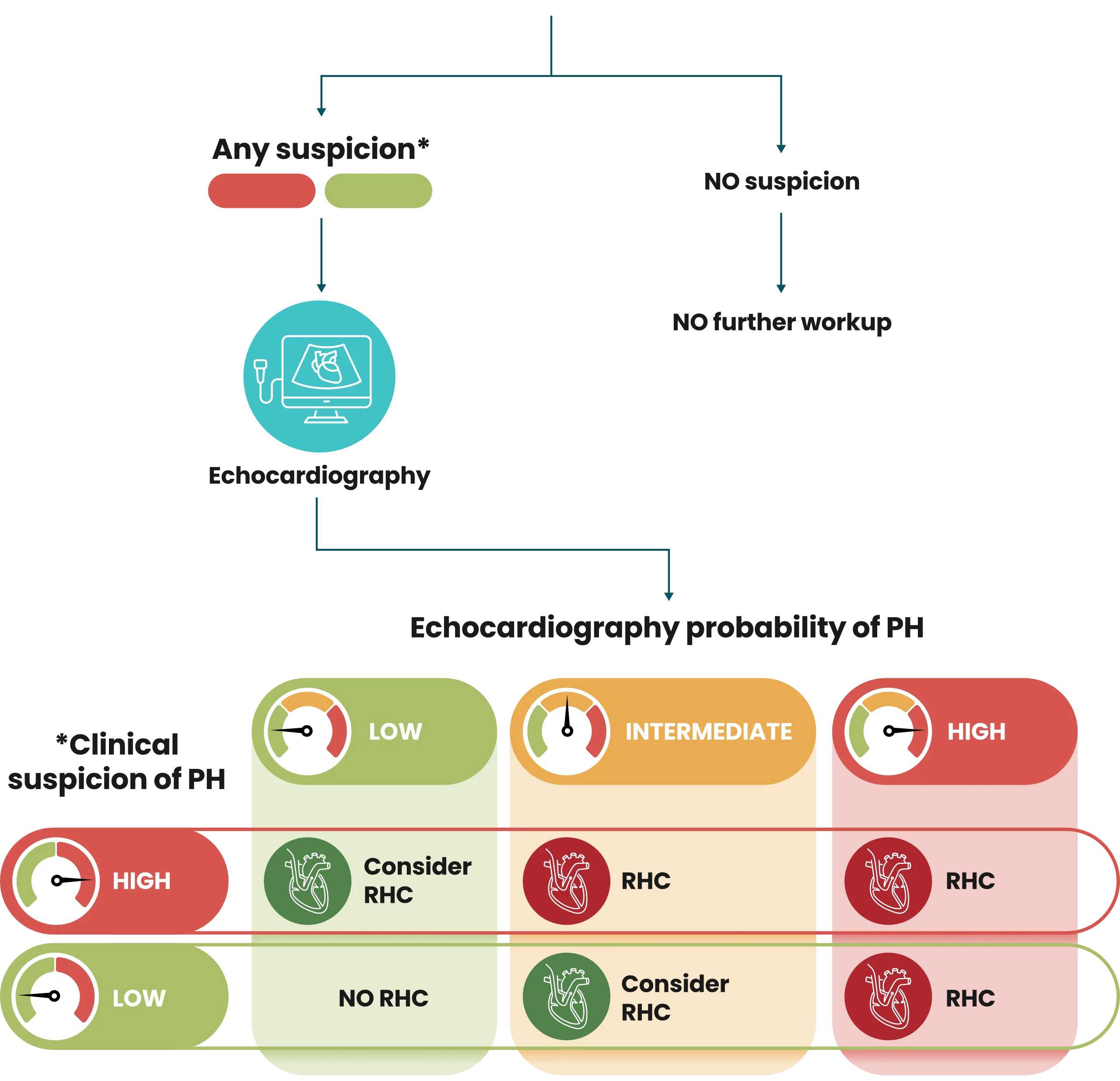
2 Initial Set of PH Screening
Panelist consensus: When PH is suspected, echocardiogram and BNP or NT-proBNP are useful as subsequent screening tests
-
Echocardiogram
-
BNP or NT-proBNP elevation brain natriuretic peptide or N-terminal pro-brain natriuretic peptide
3 Confirm a PH Diagnosis
Right heart catheterization
Clinical Process and Criteria for PH Diagnosis
Risk factors/symptoms
- History of pulmonary embolism or heart failure
- Dizziness, palpitations, syncope
Signs
- Altered heart sounds (loud P2 or S2)
- Signs of right heart failure
- Jugular venous distention
- Ankle swelling/peripheral edema
- Hepatomegaly/ascites
Diagnostic criteria used in concert to risk stratify for pulmonary hypertension
PFTs
- DLCO decline > 15%
- DLCO < 40% predicted
- Worsening FVC/ DLCO
- FVC%/ DLCO% > 1.6
Oxygen saturation & 6MWT
- Any supplemental oxygen needs
- Desaturation disproportionate to ILD severity
- Worsening desaturation
- Lower distance on 6MWT
CT scan
- RV enlargement
- PA enlargement
- PA/aorta ratio > 1.0
BNP/NT-proBNP
- Elevated BNP (> 200 pg/mL)
- Elevated NT-proBNP (> 395 pg/mL)
Individual laboratories may have different thresholds
Delphi Panel of Experts
-
Franck Rahaghi, MD Cleveland Clinic Florida Weston, FL

-
Nicholas Kolaitis, MD UCSF Health San Francisco, CA

-
Ayodeji Adegunsoye, MD The University of Chicago School of Medicine Chicago, IL

-
Joao de Andrade, MD Vanderbilt University Medical Center Nashville, TN

-
Kevin Flaherty, MD University of Michigan Health System Ann Arbor, MI

-
Lisa Lancaster, MD Vanderbilt University Medical Center Nashville, TN

-
Joyce Lee, MD University of Colorado School of Medicine Aurora, CO

-
Deborah Levine, MD Stanford University Stanford, CA

-
Ioana Preston, MD Tufts Medical Center Boston, MA

-
Zeenat Safdar, MD Houston Methodist Houston, TX

-
Rajan Saggar, MD UCLA School of Medicine Los Angeles, CA

-
Sandeep Sahay, MD Houston Methodist Houston, TX

-
Mary Beth Scholand, MD University of Utah Health Salt Lake City, UT

-
Oksana Shlobin, MD Inova Fairfax Hospital Falls Church, VA

-
David Zisman, MD Sansum Clinic Santa Barbara, CA

-
Steven Nathan, MD Inova Fairfax Hospital Falls Church, VA

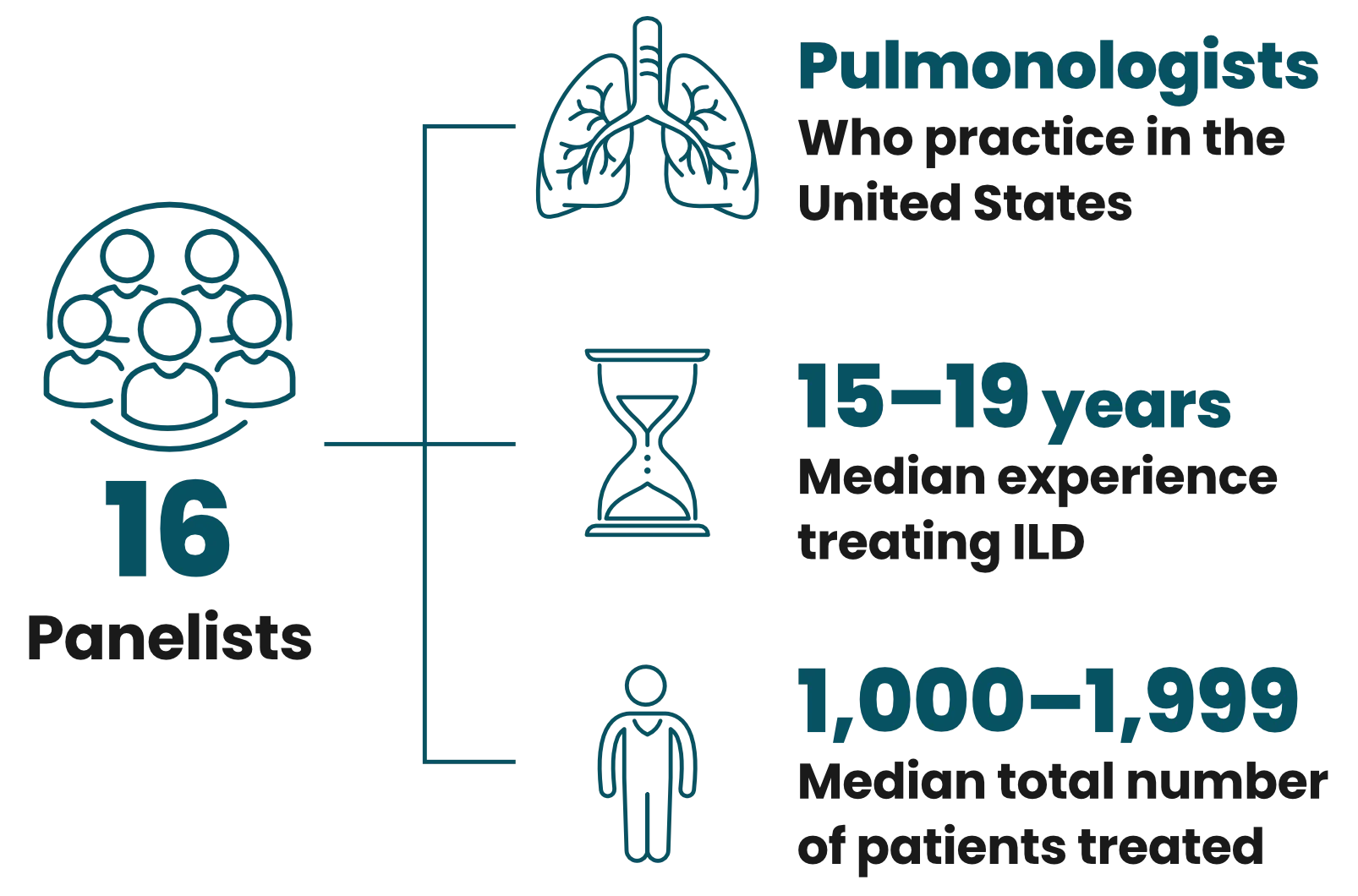
Practice settings by the numbers*
-
ILD Centers
 12
12
-
PH Centers
 8
8
-
General Pulmonology
 1
1
-
PH & ILD Centers
 2
2
* Some panelists practice in multiple settings
Method & panel selection
The modified Delphi method is a systematic approach of obtaining consensus opinions from a panel of independent experts. A PH-ILD working group convened by United Therapeutics constituted most of the Delphi panel. The remaining panelists were nominated by working group members, reviewed, and invited based on the number of nominations and diversity to ensure the Delphi panel was composed of experts from varied backgrounds and practices.
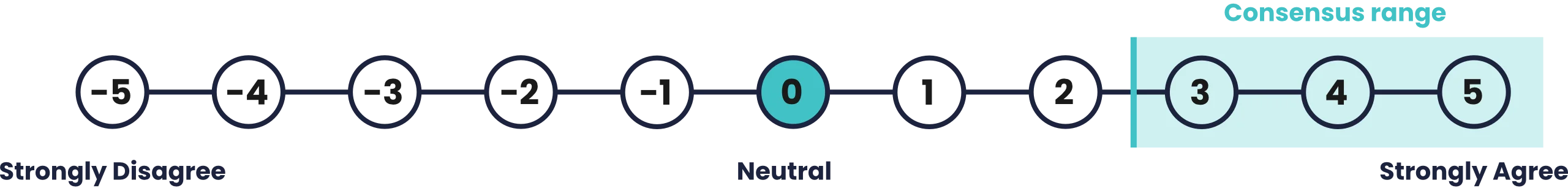
Modified Delphi Methodology
Developed and moderated by 3 expert panelists
Likert scale mean score ≥ 2.5 with standard deviation not crossing 0
5-POINT LIKERT SCALE
Survey Contents
Open questions on PH in ILD screening
-
Who would benefit from early diagnosis and treatment?
-
Test and imaging results
-
Physical signs and symptoms
-
Role of comorbidities and overall approach to screening
Statements regarding screening for PH in ILD
-
Panelists rated agreement with statements on the above Likert scale
-
Panelists could expand on responses in open-response questions
Review of the results of Survey 2
-
Panelists could reevaluate their answers with the group’s response
-
Intended to build consensus